As a practice, we are fully committed to the sustainability and reduction of our carbon footprint. We have signed up to being a ‘Greener Practice’ and will be working with both our staff and patients to improve our carbon footprint.
Green Impact For Health Toolkit
Green Inhaler
For many people with lung disease, inhalers are a lifeline; allowing you to take control of breathing problems and open up your airways. So it can come as a shock to learn that some inhalers come with a large carbon footprint. The most commonly used inhaler in the UK for instance, Ventolin Evohaler™, has a carbon footprint equivalent to 28kg of CO2. Many patients are now seeking ways to reduce the greenhouse gas released from their inhalers. For some, switching inhalers could save as much greenhouse gas as becoming vegetarian.
Equivalent tailpipe greenhouse gas emissions from a Ventolin Evohaler (containing 100 2-puff doses) and a Ventolin Accuhaler (60 1-puff doses). Assumes car achieves 100gCO2/km.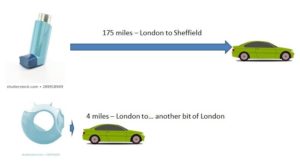
Before making any changes to your treatment you should consult a healthcare professional. Stopping your inhaler because of its carbon footprint is not recommended, not least because if you have an exacerbation the extra treatment you need could greatly increase your carbon footprint!
This site will show you why some inhalers have such a large carbon footprint and will outline some ways to reduce it. Some patients may be able to switch inhalers, but the most important thing is to keep your disease under control. If you do need an inhaler containing greenhouse gases please don’t feel guilty – everyone has a carbon footprint. There are still things you can do to reduce the carbon footprint of your inhalers, and the pharmaceutical industry is working hard to develop new propellants with a much smaller carbon footprint.
The Named GP is largely a role of oversight. It reassures patients they have one GP who is responsible for their care.
- Patients do not need to see their named GP when they book an appointment with the practice.
- Patients are entitled to choose to see any GP or nurse in the practice but please be aware you may have to wait longer.
- The named GP works with relevant health and social care professionals to deliver a multidisciplinary care package that meets the needs of the patients.
- The named GP ensures that these patients have access to a health check
- The named GP will NOT take on 24hr responsibility for the patient.
Here at Swallownest Health Centre we will invite you to an annual Health Check with one of our Physician associates, please see below for more information.
Speak up Self Advocacy, which is a charity in Rotherham for people with learning disabilities, have made a short film about Annual Health Checks to raise awareness. We think this should help ease anxieties for some people and thus increase uptake.
The video can be accessed with the following link:
https://vimeo.com/685828478/6999f8349e
Please check out Speakup's website www.speakup.org.uk for more information.
Losing a baby can be an unbelievably painful and traumatic experience.
That's why parents who have lost a baby before 24 weeks of pregnancy in England can now apply for an official baby loss certificate.
This is a voluntary service we’re introducing as part of the #WomensHealthStrategy and #PregnancyLossReview to support grieving parents and acknowledge their pain.
Information on eligibility and how to apply: https://www.gov.uk/request-baby-loss-certificate
Our practice does not offer a Blue Badge completion service, if you have been asked for supporting professional information, please contact your specialist. Blue badge parking permits – Rotherham Metropolitan Borough Council
CAMHS eClinic app is a free instant messaging service which enables young people (11-18 years) to self-refer and talk to a CAMHS Practitioner via their mobile device. Young people can download the app via android or IOS, register their details and book an appointment via the app. The appointment is held via a text message-based service.
A carer is a person who is in receipt of a carer’s allowance, or who is the main carer of an elderly or disabled person whose welfare may be at risk if the carer falls ill.
If you feel you are a carer, please complete the form here.
If you already are registered as a carer or know someone who is a carer that needs support, please see below.
Link to support services in our area - Carer Support – Rother Valley South PCN
If you are caring for one of our patients that has Dementia, Learning Disabilities or is Case managed and has a yellow care plan at home you will be offered a Carers check at the patient’s review. If you have not been offered this, please contact us and we can remedy this.
Our in-house Link Workers can also help with signposting to local services for carers ask at reception today to be referred to the Link Workers
There is a wealth of information on the NHS website about carers and caring. Below are some links into the site that we hope you will find useful.
- A guide to care and support
Information for carers and people who have care & support needs.
- Caring for someone
Advice on providing care, medicines etc.
- Care after hospital
Providing care for people who have been recently discharged from hospital.
- Taking a break
Caring for someone can be a full-time job - find out about accessing breaks and respite care.
- Support and benefits for carers
Caring for someone can be a full-time job - find out about accessing breaks and respite care.
-
Guidance, support and help with employment issues.
Advice for carers 18 or under and their entitlement to support
Contact Carers Direct
- Telephone
- 0808 802 0202
- Helpline Information
- http://www.nhs.uk/carersdirect/carerslives/updates/pages/carersdirecthelpline.aspx
- [email protected]
- Office Hours
- Lines are open 8am to 9pm Monday to Friday, 11am to 4pm at weekends. Calls are free from UK landlines.
Finance and Law
Help claiming benefits, looking after your bank balance and understanding the legal issues of caring.
- Benefits for carers
Directing carers to the benefits that can help them in their caring role
- Benefits for the under-65s
Advice and information on helping the person you look after get the benefits that they are entitled to.
Advice and information on financial support for older people with a disability or illness.
- Carer's Assement
How your benefits maybe affected after the death of the person you look after and what happens to their benefits
- Other benefits
Advice for carers and the people they are looking after on claiming a whole host of other benefits unrelated to their disability or caring
How to check your IUD Coil is in place and what to do if it is not:
Our Complaints Process
Talk to us – Every patient has the right to make a complaint about the treatment or care they have received at Swallownest Health Centre. We understand that we may not always get everything right and, by telling us about the problem you have encountered, we will be able to improve our services and patient experience.
How to complain – Please speak to a member of staff who can send you out the complaints form via text or email this form can also be found in reception as a paper copy. Alternately you can scan the QR code below or find the form/QR code on our website. Website link for our Complaints Process https://swallownesthealthcentre.co.uk/. Once you have filled in the form please return it and the complaint will be dealt with in due course. Complaint form - https://forms.office.com/e/BjeDkgbxY4
Time frames for complaints – The time constraint on bringing a complaint is 12 months from the occurrence giving rise to the complaint, or 12 months from the time you become aware of the matter about which you wish to complain. The complaints team will respond to all complaints to acknowledge them within three business days. We will aim to investigate and provide you with the findings as soon as we can and will provide updates regarding the investigation of your complaint.
Investigating complaints – Swallownest Health Centre will investigate all complaints effectively and in conjunction with extant legislation and guidance.
Confidentiality – Swallownest Health Centre will ensure that all complaints are investigated with the utmost confidentiality and that any documents are held separately from the patient’s healthcare record.
Third party complaints - Swallownest Health Centre allows a third party to make a complaint on behalf of a patient. The patient must provide consent for them to do so.
Final response - Swallownest Health Centre will issue a final formal response to all complainants which will provide full details and the outcome of the complaint. Further information is detailed in our organisation policy. If for any reason you do not want to speak to a member of our staff, then you can request that The South Yorkshire ICB (integrated care board) who provide oversight to GP surgeries investigates your complaint. They will contact us on your behalf.
South Yorkshire Integrated Care Board (ICB)
Rotherham Office
Oak House
Bramley
Rotherham
S66 1YY
Complaints number – 0114 305 1000
Advocacy support • POhWER support centre can be contacted via 0300 456 2370 • Advocacy People gives advocacy support on 0330 440 9000 • Age UK on 0800 055 6112 • Local Council can give advice on local advocacy services.
Further action - If you are dissatisfied with the outcome of your complaint from either NHS England or this organisation, then you can escalate your complaint to: Parliamentary Health Service Ombudsman (PHSO)
Parliamentary Health Service Ombudsman (PHSO)
Milbank Tower, Milbank, London, SW1P 4QP
Tel: 0345 015 4033
Book a Test or Vaccination and general advice - Coronavirus (COVID-19) - NHS (www.nhs.uk)
How to use an Oximeter at home - https://youtu.be/ldgGIOe5q9Q
To obtain a Covid vaccination certificate for Travel it is recommended to use the NHS APP which you can download to your mobile phone. Alternatively, this can be obtained either via the NHS website (see below) or by calling 119 who can post you a certificate out. This process takes around 7 days so please bear this in mind when you need to travel.
Please use this Link for further information regarding obtaining a Covid certificate.
https://www.nhs.uk/conditions/coronavirus-covid-19/covid-pass/get-your-covid-pass-letter/
Our practice does not provide Covid vaccination certificates or letters.
Please be advised that the surgery does not provide Covid Recovery letters for travel. If you have tested positive and are using the NHS App, your COVID passport will not be available for at least 14 days post the date you were confirmed as having a positive test result. Once the 14 days have passed your COVID pass should become available again for you to download and this will show the covid recovery proof in such cases. Please Call 119 or visit the Government website for information on Using your NHS COVID Pass for travel abroad and at venues and settings in England – this guidance is regularly updated. We are aware certain countries want an additional letter via a health professional for travel separate to the NHS covid pass recovery letter. Unfortunately, this Non-NHS service is not something we currently provide as you can appreciate, we do not want to reduce and divert GP and administrative capacity for NHS services at the practice. Please do not contact the surgery for such letters, as we are unable to help. There are private providers who can arrange this online.
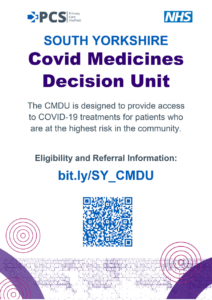 The South Yorkshire COVID Medicines Decision Unit is operational and designed to provide access to COVID-19 treatments for patients at the highest risk in the community, as advised by NHS England.
The South Yorkshire COVID Medicines Decision Unit is operational and designed to provide access to COVID-19 treatments for patients at the highest risk in the community, as advised by NHS England.
To find out more, visit: https://southyorkshire.icb.nhs.uk/your-health/accessing-covid-19-treatment-risk-patients
Swallownest Health Centre is a Dementia Friendly practice. We have pledged to work towards providing a safe and caring environment for patients with dementia. Our first step towards this goal is providing training for all our staff so that we are all aware of the day to day problems faced by people with dementia.
We have also created this page on our website which we hope to develop as new information is obtained.
We also recognise that the people caring for people with dementia sometimes need information and support. To access information please click on the link below.
Carers Information and Support Programme
Click on the following link for fact sheets about Alzheimer's
Swallownest Health Centre is proud to have signed up to become Dementia Friendly.
We will be working with Alzheimer’s Society during the coming year and our staff have been trained and will also be participating in General Practice specific dementia awareness sessions.
We will also be carrying out an assessment of how dementia-friendly we are and take steps to improve areas that need attention.We welcome any feedback about how we are doing from patients, families and carers.
Included here are some useful contacts and links for support or advice if you are living with dementia or caring for someone with dementia.
Alzheimer’s Society Dementia Adviser Service: Tel: 01332 208845
Alzheimer’s Society website (for anyone affected by dementia): https://www.alzheimers.org.uk/
Dementia Connect: https://www.alzheimers.org.uk/info/20011/find_support_near_you#!/search
National Dementia Helpline: 0300 222 11 22
Alzheimer's Society
From day one of dementia, we'll be right here with you. For support and advice. For pushing for change, and for life-changing treatments and care.
- Early Help and Social Care – Rotherham SEND Local Offer Early Help and Social Care teams work with children, young people, and their families to offer advice and support when problems first emerge.
- Welcome to Rotherham CAMHS – CAMHS (rdash.nhs.uk) – support for children w/ mental health issues.
- Refer to Single Point of Access | Instructions – Rotherham Metropolitan Borough Council to report any social concerns.
Easy as 1, 2, 3!
1. Receive Appointment Times
2. Give Firefly a Call
3. We Pick You Up & Take Away the Stress!!
Further information can be obtained via the website or contact:
07738 390541
www.firefly-support.co.uk
Our Practice does not offer a Fit2Fly form/certificate completion service they can be obtained through a Private GP service.
Flu Campaign 2022/23
Information about flu vaccine supplies.
People who are most at risk from the complications of flu are recommended to get a flu vaccine every year. This winter it is especially important with flu and coronavirus (COVID-19) both in circulation. Research shows that if you get both at the same time you may be more seriously ill.
Vaccine administering is restricted to patients who are eligible only. Please refer to the Government link here to find out more https://www.gov.uk/government/publications/flu-vaccines-for-the-current-season/flu-vaccines-for-the-2022-to-2023-season#eligible-groups
The eligible groups are as follows (in line with Government guidance)
- aged 2 and 3 years on 31 August 2022
- school aged children (all primary school aged children (reception year to year 6) and eligible secondary school aged children)
- those aged 6 months to under 50 years in clinical risk groups
- pregnant women
- Healthy 50 to 64-year olds (Strict guidance is that this cohort will not be offered this until after 15 October 2022)
- all those aged 65 years and over
- those in long-stay residential care homes
- carers / in receipt of carer’s allowance / or main carer of an older or disabled person
- close contacts of immunocompromised individuals
- frontline health and social care staff
Why should I have my flu vaccine at my GP? Swallownest Health Centre supports you as our patient, and as such a flu vaccine has already been ordered (in September 2021) for all our registered patients who are eligible to receive one. Therefore, if you fall within any of the eligible categories, we will actually have a vaccine with your name on (so to speak). We have to do this and assure NHS England we have enough vaccines for everyone. We have to buy the vaccines for you and we can only return limited numbers that go unused, and the rest have to paid for by the surgery. Please come to receive your vaccination with us, YOUR local GP surgery, we have bought your vaccine and want to protect you!
We operate as an independent and individual organisation, and therefore are not working in association with any other organisation in offering flu vaccines. We offer a setting where we can check your medical records and documented allergies and make sure you get the most suitable vaccine. We also have medical staff at hand, all of which help with safe administering of your vaccine.
We can offer protection for those who may be forgetful by reducing the risk of duplication in vaccines being administered
We offer a fast, efficient and friendly flu clinic service with your local surgery team (and we really enjoy our drop-in flu clinic sessions, it gives us a nice break from our ‘normal’ work)
We can ensure continuity of care for our patients and carers (we know you already).
How do I make my appointment? We don’t add clinics to our clinical system until our vaccines have been delivered and are in our fridges. At which point we will add and will be sending out text messages where you can click on the link to book an appointment. You don’t need to be signed up to online access to do this. We did last year, and it was a success and also eases any burden on our phone lines. Please note that we will not send text messages to everyone at once. We will do this in stages in line with our clinics available, so please be patient.
Can I make a call or visit the health centre to book an appointment for my flu vaccine? Yes you can, we would recommend that you contact us after 2pm if you need to call to book, as our phone lines are quieter at this time. Please note that appointments will not all be added at once, we will be adding in stages whilst we monitor our stock, staffing and other duties. We will do our best to provide a variety of appointments including early morning and later afternoons to support patient access. We are looking to have 2 weekend dates also.
I have an appointment at the Health Centre for something else, can I have my vaccine whilst I am there? Yes of course if the clinician has the time and if you are eligible. Please check with the clinician.
What will happen when I arrive? Please prepare by removing any coats or jumpers. This will make the process easier and quicker for all.
How is this different to normal? We are conducting our flu clinics the way that we have the last couple of years, as this has worked really well for us and our patients. We will be having 2 weekend dates (TBC) and we will also have a variety of appointments during the day with Healthcare Assistants.
What do I need to do? We would recommend that you wear a face mask to protect any vulnerable patients and staff, ensure you wash your hands before and after, DO NOT attend if you or a close contact have symptoms or have had contact with a suspected/confirmed case of Covid.
What about car parking? To ease the pressure in the car park, if you are able to walk to the centre, we would strongly advise you to.
How long will it take? Appointments are very quick, and you will be asked a couple of questions by the clinician to enable them to know if you are ok to have the vaccine.
Will I just be offered my flu vaccination? We are unable to offer covid vaccinations here, however we can confirm that they are being offered at Anston, amongst many other sites. Appointments for these are available on the National Booking Service https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/book-coronavirus-vaccination/ Please note that you are able to have Covid and flu vaccinations on the same day as it is completely safe. We would also be able to offer you the pneumonia vaccine if you are eligible and haven’t already had it. https://www.nhs.uk/conditions/vaccinations/pneumococcal-vaccination/
We regularly contact patients with regards to pneumonia and also shingles vaccines. We do not administer shingles vaccines with our flu vaccines.
What do I do after I’ve had my vaccination? Following your vaccine, you should be able to leave immediately.
Not eligible for NHS flu vaccination? Unfortunately, we are not able to give flu vaccinations to patients who are not eligible under the NHS programme. However, you are able to pay get the flu vaccination at a pharmacy.
Housebound patients
We have a team who will be supporting us in our housebound flu vaccines. You do not need to do anything to trigger your flu vaccination. You will be contacted by the team who will be administering these. These will begin in September. Your GP knows which patients are housebound.
Childrens Nasal Flu
Please note that we are shortly be inviting all eligible children for the Nasal Flu, unfortunately we are only allowed to order in stages so have to limit the number of invitations we send out at any one time. Please DO NOT contact the surgery to enquire we will be contacting the parents of Children who are eligible in due course. If your child has received theirs at school or you wish to decline, please let us know so we can offer to another child.
Should you wish to read more regarding facts about flu and the flu vaccine, please copy and paste the link below into your browser https://www.nhs.uk/conditions/vaccinations/flu-influenza-vaccine/
We would like to thank you for your continued co-operation, understanding and support.
Swallownest Health Centre
There has never been a more important time to KEEP MOVING!!
Functional fitness has a range of programmes to support people. They offer cancer rehab, falls prevention, weight management, stroke exercise rehab and much much more. You can get all the information by calling 07740 188 212 or by visiting the website.
Introduction:
This privacy notice lets you know what happens to any personal data that you give to us, or any that we may collect from or about you.
This privacy notice applies to personal information processed by or on behalf of the practice.
This Notice explains
-
- Who we are, how we use your information and our Data Protection Officer
-
- What kinds of personal information about you do we process?
-
- What are the legal grounds for our processing of your personal information (including when we share it with others)?
-
- What should you do if your personal information changes?
-
- For how long your personal information is retained by us?
-
- What are your rights under data protection laws?
The General Data Protection Regulation (GDPR) became law on 24th May 2016. This is a single EU-wide regulation on the protection of confidential and sensitive information. It enters into force in the UK on the 25th May 2018, repealing the Data Protection Act (1998).
For the purpose of applicable data protection legislation (including but not limited to the General Data Protection Regulation (Regulation (EU) 2016/679) (the "GDPR"), and the Data Protection Act 2018 (currently in Bill format before Parliament) the practice responsible for your personal data is Dr Clarke & Partners
This Notice describes how we collect, use and process your personal data, and how, in doing so, we comply with our legal obligations to you. Your privacy is important to us, and we are committed to protecting and safeguarding your data privacy rights
How we use your information and the law.
Swallownest Health Centre will be what’s known as the ‘Controller’ of the personal data you provide to us.
We collect basic personal data about you which does not include any special types of information or location-based information. This does however include name, address, contact details such as email and mobile number etc.
We will also collect sensitive confidential data known as “special category personal data”, in the form of health information, religious belief (if required in a healthcare setting) ethnicity, and sex during the services we provide to you and or linked to your healthcare through other health providers or third parties.
Why do we need your information?
The Health Care Professionals who provide you with care maintain records about your health and any treatment or care you have received previously (e.g. NHS Trust, GP Surgery, Walk-in clinic, etc.). These records help to provide you with the best possible healthcare.
NHS health records may be electronic, on paper or a mixture of both, and we use a combination of working practices and technology to ensure that your information is kept confidential and secure. Records which the Practice hold about you may include the following information;
-
- Details about you, such as your address, carer, legal representative, emergency contact details
-
- Any contact the surgery has had with you, such as appointments, clinic visits, emergency appointments, etc.
-
- Notes and reports about your health
-
- Details about your treatment and care
-
- Results of investigations such as laboratory tests, x-rays etc
-
- Relevant information from other health professionals, relatives or those who care for you
To ensure you receive the best possible care, your records are used to facilitate the care you receive. Information held about you may be used to help protect the health of the public and to help us manage the NHS. Information may be used within the GP practice for clinical Audit to monitor the quality of the service provided.
How do we lawfully use your data?
We need to know your personal, sensitive and confidential data in order to provide you with Healthcare services as a General Practice, under the General Data Protection Regulation we will be lawfully using your information in accordance with: -
Article 6, e) processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller;”
Article 9, (h) processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems
This Privacy Notice applies to the personal data of our patients and the data you have given us about your carers/family members.
Risk Stratification
Risk stratification data tools are increasingly being used in the NHS to help determine a person’s risk of suffering a condition, preventing an unplanned or (re)admission and identifying a need for preventive intervention. Information about you is collected from a number of sources including NHS Trusts and from this GP Practice. A risk score is then arrived at through an analysis of your de-identified information is only provided back to your GP as data controller in an identifiable form. Risk stratification enables your GP to focus on preventing ill health and not just the treatment of sickness. If necessary, your GP may be able to offer you additional services. Please note that you have the right to opt out of your data being used in this way.
Medicines Management
The Practice may conduct Medicines Management Reviews of medications prescribed to its patients. This service performs a review of prescribed medications to ensure patients receive the most appropriate, up to date and cost-effective treatments.
Safeguarding
The Practice is dedicated to ensuring that the principles and duties of safeguarding adults and children are holistically, consistently and conscientiously applied with the wellbeing of all, at the heart of what we do.
Our legal basis for processing For the General Data Protection Regulation (GDPR) purposes is: -
Article 6(1)(e) ‘…exercise of official authority…’.
For the processing of special categories data, the basis is: -
Article 9(2)(b) – ‘processing is necessary for the purposes of carrying out the obligations and exercising specific rights of the controller or of the data subject in the field of employment and social security and social protection law…’
Categories of personal data
The data collected by Practice staff in the event of a safeguarding situation will be as much personal information as is necessary or possible to obtain in order to handle the situation. In addition to some basic demographic and contact details, we will also process details of what the safeguarding concern is. This is likely to be special category information (such as health information).
Sources of the data
The Practice will either receive or collect information when someone contacts the organisation with safeguarding concerns or we believe there may be safeguarding concerns and make enquiries to relevant providers.
Recipients of personal data
The information is used by the Practice when handling a safeguarding incident or concern. We may share information accordingly to ensure duty of care and investigation as required with other partners such as local authorities, the police or healthcare professionals (i.e. their GP or mental health team).
How do we maintain the confidentiality of your records?
We are committed to protecting your privacy and will only use information collected lawfully in accordance with:
-
- Data Protection Act 2018
-
- The General Data Protection Regulations 2016
-
- Human Rights Act 1998
-
- Common Law Duty of Confidentiality
-
- Health and Social Care Act 2012
-
- NHS Codes of Confidentiality, Information Security and Records Management
-
- Information: To Share or Not to Share Review
Every member of staff who works for an NHS organisation has a legal obligation to keep information about you confidential.
We will only ever use or pass on information about you if others involved in your care have a genuine need for it. We will not disclose your information to any third party without your permission unless there are exceptional circumstances (i.e. life or death situations), where the law requires information to be passed on and / or in accordance with the information sharing principle following Dame Fiona Caldicott’s information sharing review (Information to share or not to share) where “The duty to share information can be as important as the duty to protect patient confidentiality.” This means that health and social care professionals should have the confidence to share information in the best interests of their patients within the framework set out by the Caldicott principles.
Our practice policy is to respect the privacy of our patients, their families and our staff and to maintain compliance with the General Data Protection Regulations (GDPR) and all UK specific Data Protection Requirements. Our policy is to ensure all personal data related to our patients will be protected.
All employees and sub-contractors engaged by our practice are asked to sign a confidentiality agreement. The practice will, if required, sign a separate confidentiality agreement if the client deems it necessary. If a sub-contractor acts as a data processor for an appropriate contract (art 24-28) will be established for the processing of your information.
In Certain circumstances you may have the right to withdraw your consent to the processing of data. Please contact the Data Protection Officer in writing if you wish to withdraw your consent. If some circumstances we may need to store your data after your consent has been withdrawn to comply with a legislative requirement.
Some of this information will be held centrally and used for statistical purposes. Where we do this, we take strict measures to ensure that individual patients cannot be identified. Sometimes your information may be requested to be used for research purposes – the surgery will always gain your consent before releasing the information for this purpose in an identifiable format. In some circumstances you can Opt-out of the surgery sharing any of your information for research purposes.
With your consent we would also like to use your information to
We would however like to use your name, contact details and email address to inform you of services that may benefit you, with your consent only. There may be occasions were authorised research facilities would like you to take part on innovations, research, improving services or identifying trends.
At any stage where we would like to use your data for anything other than the specified purposes and where there is no lawful requirement for us to share or process your data, we will ensure that you have the ability to consent and opt out prior to any data processing taking place.
This information is not shared with third parties or used for any marketing and you can unsubscribe at any time via phone, email or by informing the practice DPO as below.
Where do we store your information Electronically?
All the personal data we process is processed by our staff in the UK however for the purposes of IT hosting and maintenance this information may be located on servers within the European Union.
No 3rd parties have access to your personal data unless the law allows them to do so and appropriate safeguards have been put in place. We have a Data Protection regime in place to oversee the effective and secure processing of your personal and or special category (sensitive, confidential) data.
Who are our partner organisations?
We may also have to share your information, subject to strict agreements on how it will be used, with the following organisations;
-
- NHS Trusts / Foundation Trusts
-
- GP’s
-
- NHS Commissioning Support Units
-
- Independent Contractors such as dentists, opticians, pharmacists
-
- Private Sector Providers
-
- Voluntary Sector Providers
-
- Ambulance Trusts
-
- Clinical Commissioning Groups
-
- Social Care Services
-
- NHS England (NHSE) and NHS Digital (NHSD)
-
- Multi Agency Safeguarding Hub (MASH)
-
- Local Authorities
-
- Education Services
-
- Fire and Rescue Services
-
- Police & Judicial Services
-
- Voluntary Sector Providers
-
- Private Sector Providers
-
- Other ‘data processors’ which you will be informed of
You will be informed who your data will be shared with and in some cases asked for consent for this to happen when this is required.
Computer System This practice operates a Clinical Computer System on which NHS Staff record information securely. This information can then be shared with other clinicians so that everyone caring for you is fully informed about your medical history, including allergies and medication.
To provide around the clock safe care, unless you have asked us not to, we will make information available to trusted organisations. Wherever possible, their staff will ask your consent before your information is viewed.
We consider patient consent as being the key factor in dealing with your health information.
Shared Care Records
To support your care and improve the sharing of relevant information to our partner organisations when they are involved in looking after you, we will share information to other systems. The general principle is that information is passed to these systems unless you request this does not happen, but that system users should ask for your consent before viewing your record.
We may also use external companies to process personal information, such as for archiving purposes. These companies are bound by contractual agreements to ensure information is kept confidential and secure. All employees and sub-contractors engaged by our practice are asked to sign a confidentiality agreement. If a sub-contractor acts as a data processor for Dr Clarke & Partners an appropriate contract (art 24-28) will be established for the processing of your information.
Sharing your information without consent
We will normally ask you for your consent, but there are times when we may be required by law to share your information without your consent, for example:
-
- where there is a serious risk of harm or abuse to you or other people;
-
- where a serious crime, such as assault, is being investigated or where it could be prevented;
-
- notification of new births;
-
- where we encounter infectious diseases that may endanger the safety of others, such as Meningitis or measles (but not HIV/AIDS);
-
- where a formal court order has been issued;
-
- where there is a legal requirement, for example if you had committed a Road Traffic Offence.
How long will we store your information?
We are required under UK law to keep your information and data for the full retention periods as specified by the NHS Records management code of practice for health and social care and national archives requirements.
More information on records retention can be found online at (https://digital.nhs.uk/article/1202/Records-Management-Code-of-Practice-for-Health-and-Social-Care-2016 )
How can you access, amend move the personal data that you have given to us?
Even if we already hold your personal data, you still have various rights in relation to it. To get in touch about these, please contact us. We will seek to deal with your request without undue delay, and in any event in accordance with the requirements of any applicable laws. Please note that we may keep a record of your communications to help us resolve any issues which you raise.
Right to object: If we are using your data because we deem it necessary for our legitimate interests to do so, and you do not agree, you have the right to object. We will respond to your request within 30 days (although we may be allowed to extend this period in certain cases). Generally, we will only disagree with you if certain limited conditions apply.
Right to withdraw consent: Where we have obtained your consent to process your personal data for certain activities (for example for a research project), or consent to market to you, you may withdraw your consent at any time.
Right to erasure: In certain situations (for example, where we have processed your data unlawfully), you have the right to request us to "erase" your personal data. We will respond to your request within 30 days (although we may be allowed to extend this period in certain cases) and will only disagree with you if certain limited conditions apply. If we do agree to your request, we will Delete your data but will generally assume that you would prefer us to keep a note of your name on our register of individuals who would prefer not to be contacted. That way, we will minimise the chances of you being contacted in the future where your data are collected in unconnected circumstances. If you would prefer us not to do this, you are free to say so.
Right of data portability: If you wish, you have the right to transfer your data from us to another data controller. We will help with this with a GP to GP data transfer and transfer of your hard copy notes.
Access to your personal information
Data Subject Access Requests (DSAR): You have a right under the Data Protection legislation to request access to view or to obtain copies of what information the surgery holds about you and to have it amended should it be inaccurate. To request this, you need to do the following:
-
- Your request should be made to the Practice – for information from the hospital you should write direct to them
-
- There is no charge to have a copy of the information held about you
-
- We are required to respond to you within one month
-
- You will need to give adequate information (for example full name, address, date of birth, NHS number and details of your request) so that your identity can be verified, and your records located information we hold about you at any time.
What should you do if your personal information changes?
You should tell us so that we can update our records please contact the Practice Manager as soon as any of your details change, this is especially important for changes of address or contact details (such as your mobile phone number), the practice will from time to time ask you to confirm that the information we currently hold is accurate and up-to-date.
Objections / Complaints
Should you have any concerns about how your information is managed at the GP, please contact the GP Practice Manager or the Data Protection Officer as above. If you are still unhappy following a review by the GP practice, you have a right to lodge a complaint with a supervisory authority: You have a right to complain to the UK supervisory Authority as below.
Information Commissioner:
Wycliffe house
Water Lane
Wilmslow
Cheshire
SK9 5AF
Tel: 01625 545745
If you are happy for your data to be extracted and used for the purposes described in this privacy notice, then you do not need to do anything. If you have any concerns about how your data is shared, then please contact the Practice Data Protection Officer.
If you would like to know more about your rights in respect of the personal data we hold about you, please contact the Data Protection Officer as below.
Data Protection Officer:
The Practice Data Protection Officer is Paul Couldrey of PCIG Consulting Limited. Any queries regarding Data Protection issues should be addressed to him at: -
Email: [email protected]
Postal: PCIG Consulting Limited
7 Westacre Drive
Quarry Bank
Dudley
West Midlands
DY5 2EE
Changes:
It is important to point out that we may amend this Privacy Notice from time to time. If you are dissatisfied with any aspect of our Privacy Notice, please contact the Practice Data Protection Officer.
If you need help with any of the below, please follow this link: www.sybhealthiertogether.nhs.uk
- Advice for families and young people on what 'red-flag' signs to look out for
- Where to seek help if required
- What to do to keep an unwell child comfortable
- How long symptoms should last, for a wide range of health conditions, including rashes, coughs, asthma, bronchiolitis, fever and many others
To visit the Healthwatch website and rate our service please click on the link below
If you’re more than 10 weeks pregnant or have a child under 4, you may be entitled to get help to buy healthy food and milk.
If you’re eligible, you’ll be sent a Healthy Start card with money on it that you can use in some UK shops. We’ll add your benefit onto this card every 4 weeks.
You can use your card to buy:
- plain liquid cow’s milk
- fresh, frozen, and tinned fruit and vegetables
- fresh, dried, and tinned pulses
- infant formula milk based on cow’s milk
You can also use your card to collect:
- Healthy Start vitamins – these support you during pregnancy and breastfeeding
- vitamin drops for babies and young children – these are suitable from birth to
- 4 years old
Applying online
If you get Universal credit, you can apply online if:
- you’re at least 10 weeks pregnant or have at least one child under 4 years old
- your family’s monthly ‘take-home pay for this period’ is £408 or less from employment
If you get Child Tax Credit, you can apply online if:
- you have at least one child under 4 years old
- your family’s annual income is £16,190 or less
To apply, you’ll need your:
- name
- address
- date of birth
- National Insurance number
- baby’s due date (if you’re pregnant)
- benefit award letter if you’re over 18 (you must enter the same information that’s on this letter)
Everybody in the world has mental health. Everyone.
Yet the fear of being judged is preventing many people from talking about it. At Chasing the Stigma we want to help remove that fear and unnecessary stigma, by using our own first-hand experiences to say ‘I have suffered. I got through it and you can too’. You are never alone.
If you need someone to talk to, please check the following link to the Hub of Hope - There's always someone to talk to who can help, even locally. If you click on 'talk' this will connect you straight through to chat online.
To find out more please click the link here https://www.itv.com/news/granada/2017-07-05/hub-of-hope-launch-of-mental-health-website-which-says-where-to-get-help/
In the unfortunate event that a person has passed away, there are three things that must be done in the first few days;
- Get a medical certificate from your GP or hospital doctor (this is necessary to register the death)
- Register the death within 5 days (8 days in Scotland). You will then receive the necessary documents for the funeral.
- Make the necessary funeral arrangements.
Register the death
If the death has been reported to the coroner (or Procurator Fiscal in Scotland) they must give permission before registering the death.
You can register the death if you are a relative, a witness to the death, a hospital administrator or the person making the arrangements with the funeral directors.
You can use the ‘Register a Death’ page on the gov.uk website that will guide you through the process. This will also explain the registration process for Scotland and Northern Ireland.
Arrange the funeral
The funeral can usually only take place after the death is registered. Most people use a funeral director, though you can arrange a funeral yourself.
Funeral directors
Choose a funeral director who’s a member of one of the following:
These organisations have codes of practice - they must give you a price list when asked.
Some local councils run their own funeral services, for example for non-religious burials. The British Humanist Association can also help with non-religious funerals.
Arranging the funeral yourself
Contact the Cemeteries and Crematorium Department of your local council to arrange a funeral yourself.
Funeral costs
Funeral costs can include:
- funeral director fees
- things the funeral director pays for on your behalf (called ‘disbursements’ or ‘third-party costs’), for example, crematorium or cemetery fees, or a newspaper announcement about the death
- local authority burial or cremation fees
Funeral directors may list all these costs in their quotes.
Long-term pain medication isn't your only option and can be dangerous if taken for a long time. Speak to your GP for a follow up appointment and other options available to you.
NHS Digital Data Collection from the Practice
The NHS needs data about the patients it treats to plan and deliver its services and to ensure that care and treatment provided is safe and effective. The General Practice Data for Planning and Research data collection will help the NHS to improve health and care services for everyone by collecting patient data that can be used to do this. For example patient data can help the NHS to:
- monitor the long-term safety and effectiveness of care
- plan how to deliver better health and care services
- prevent the spread of infectious diseases
- identify new treatments and medicines through health research
GP practices already share patient data for these purposes, but this new data collection will be more efficient and effective.
This means that GPs can get on with looking after their patients, and NHS Digital can provide controlled access to patient data to the NHS and other organisations who need to use it, to improve health and care for everyone.
Contributing to research projects will benefit us all as better and safer treatments are introduced more quickly and effectively without compromising your privacy and confidentiality.
NHS Digital has engaged with the British Medical Association (BMA), Royal College of GPs (RCGP) and the National Data Guardian (NDG) to ensure relevant safeguards are in place for patients and GP practices.
NHS Digital purposes for processing patient data
Patient data from GP medical records kept by GP practices in England is used every day to improve health, care and services through planning and research, helping to find better treatments and improve patient care. The NHS is introducing an improved way to share this information - called the General Practice Data for Planning and Research data collection.
NHS Digital will collect, analyse, publish and share this patient data to improve health and care services for everyone. This includes:
- informing and developing health and social care policy
- planning and commissioning health and care services
- taking steps to protect public health (including managing and monitoring the coronavirus pandemic)
- in exceptional circumstances, providing you with individual care
- enabling healthcare and scientific research
Any data that NHS Digital collects will only be used for health and care purposes. It is never shared with marketing or insurance companies.
What patient data NHS Digital collect
This collection will start from 1 July 2021. Patient data will be collected from GP medical records about:
- any living patient registered at a GP practice in England when the collection started - this includes children and adults
- any patient who died after the data collection started, and was previously registered at a GP practice in England when the data collection started
We will not collect your name or where you live. Any other data that could directly identify you, for example NHS number, General Practice Local Patient Number, full postcode and date of birth, is replaced with unique codes which are produced by de-identification software before the data is shared with NHS Digital.
This process is called pseudonymisation and means that no one will be able to directly identify you in the data. The diagram below helps to explain what this means. Using the terms in the diagram, the data we collect would be described as de-personalised.
Image provided by Understanding Patient Data under licence.
NHS Digital will be able to use the same software to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason. Only NHS Digital has the ability to do this. This would mean that the data became personally identifiable data in the diagram above. An example would be where you consent to your identifiable data being shared with a research project or clinical trial in which you are participating, as they need to know the data is about you.
More information about when we may be able to re-identify the data is in the who we share your patient data with section below.
The Data NHD Digital collect
We will only collect structured and coded data from patient medical records that is needed for specific health and social care purposes explained above.
Data that directly identifies you as an individual patient, including your NHS number, General Practice Local Patient Number, full postcode, date of birth and if relevant date of death, is replaced with unique codes produced by de-identification software before it is sent to NHS Digital. This means that no one will be able to directly identify you in the data.
NHS Digital will be able to use the software to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason. This would mean that the data became personally identifiable in the diagram above. It will still be held securely and protected, including when it is shared by NHS Digital.
NHS Digital will collect
- data on your sex, ethnicity and sexual orientation
- clinical codes and data about diagnoses, symptoms, observations, test results, medications, allergies, immunisations, referrals and recalls, and appointments, including information about your physical, mental and sexual health
- data about staff who have treated you
More detailed information about the patient data we collect is contained in the Data Provision Notice issued to GP practices.
NHS Digital Does not collect.
- your name and address (except for your postcode in unique coded form)
- written notes (free text), such as the details of conversations with doctors and nurses
- images, letters and documents
- coded data that is not needed due to its age – for example medication, referral and appointment data that is over 10 years old
- coded data that GPs are not permitted to share by law – for example certain codes about IVF treatment, and certain information about gender re-assignment
Opting out of NHS Digital collecting your data (Type 1 Opt-out)
If you do not want your identifiable patient data (personally identifiable data in the diagram above) to be shared outside of your GP practice for purposes except for your own care, you can register an opt-out with your GP practice. This is known as a Type 1 Opt-out.
Type 1 Opt-outs were introduced in 2013 for data sharing from GP practices, but may be discontinued in the future as a new opt-out has since been introduced to cover the broader health and care system, called the National Data Opt-out. If this happens people who have registered a Type 1 Opt-out will be informed. More about National Data Opt-outs is in the section Who we share patient data with.
NHS Digital will not collect any patient data for patients who have already registered a Type 1 Opt-out in line with current policy. If this changes patients who have registered a Type 1 Opt-out will be informed.
If you do not want your patient data shared with NHS Digital, you can register a Type 1 Opt-out with your GP practice. You can register a Type 1 Opt-out at any time. You can also change your mind at any time and withdraw a Type 1 Opt-out.
Data sharing with NHS Digital will start on 1 July 2021.
If you have already registered a Type 1 Opt-out with your GP practice your data will not be shared with NHS Digital.
If you wish to register a Type 1 Opt-out with your GP practice before data sharing starts with NHS Digital, this should be done by returning this form to your GP practice by 23 June 2021 to allow time for processing it. If you have previously registered a Type 1 Opt-out and you would like to withdraw this, you can also use the form to do this. You can send the form by post or email to your GP practice or call 0300 3035678 for a form to be sent out to you.
If you register a Type 1 Opt-out after your patient data has already been shared with NHS Digital, no more of your data will be shared with NHS Digital. NHS Digital will however still hold the patient data which was shared with us before you registered the Type 1 Opt-out.
If you do not want NHS Digital to share your identifiable patient data (personally identifiable data in the diagram above) with anyone else for purposes beyond your own care, then you can also register a National Data Opt-out. There is more about National Data Opt-outs and when they apply in the National Data Opt-out section below.
NHS Digital legal basis for collecting, analysing and sharing patient data.
When we collect, analyse, publish and share patient data, there are strict laws in place that we must follow. Under the UK General Data Protection Regulation (GDPR), this includes explaining to you what legal provisions apply under GDPR that allows us to process patient data. The GDPR protects everyone's data.
NHS Digital has been directed by the Secretary of State for Health and Social Care under the General Practice Data for Planning and Research Directions 2021 to collect and analyse data from GP practices for health and social care purposes including policy, planning, commissioning, public health and research purposes.
NHS Digital is the controller of the patient data collected and analysed under the GDPR jointly with the Secretary of State for Health and Social Care.
All GP practices in England are legally required to share data with NHS Digital for this purpose under the Health and Social Care Act 2012 (2012 Act). More information about this requirement is contained in the Data Provision Notice issued by NHS Digital to GP practices.
NHS Digital has various powers to publish anonymous statistical data and to share patient data under sections 260 and 261 of the 2012 Act. It also has powers to share data under other Acts, for example the Statistics and Registration Service Act 2007.
Regulation 3 of the Health Service (Control of Patient Information) Regulations 2002 (COPI) also allow confidential patient information to be used and shared appropriately and lawfully in a public health emergency. The Secretary of State has issued legal notices under COPI (COPI Notices) requiring NHS Digital, NHS England and Improvement, arm's-length bodies (such as Public Health England), local authorities, NHS trusts, clinical commissioning groups and GP practices to share confidential patient information to respond to the COVID-19 outbreak. Any information used or shared during the COVID-19 outbreak will be limited to the period of the outbreak unless there is another legal basis to use confidential patient information.
The legal basis under GDPR for General Practice Data for Planning and Research
How NHS Digital use patient data
NHS Digital will analyse and link the patient data we collect with other patient data we hold to create national data sets and for data quality purposes.
NHS Digital will be able to use the de-identification software to convert the unique codes back to data that could directly identify you in certain circumstances for these purposes, where this is necessary and where there is a valid legal reason. There are strict internal approvals which need to be in place before we can do this and this will be subject to independent scrutiny and oversight by the Independent Group Advising on the Release of Data (IGARD).
These national data sets are analysed and used by NHS Digital to produce national statistics and management information, including public dashboards about health and social care which are published. We never publish any patient data that could identify you. All data we publish is anonymous statistical data.
For more information about data we publish see Data and Information and Data Dashboards.
We may also carry out analysis on national data sets for data quality purposes and to support the work of others for the purposes set out in Our purposes for processing patient data section above.
Who NHS Digital share patient data with
All data which is shared by NHS Digital is subject to robust rules relating to privacy, security and confidentiality and only the minimum amount of data necessary to achieve the relevant health and social care purpose will be shared.
All requests to access patient data from this collection, other than anonymous aggregate statistical data, will be assessed by NHS Digital’s Data Access Request Service, to make sure that organisations have a legal basis to use the data and that it will be used safely, securely and appropriately.
These requests for access to patient data will also be subject to independent scrutiny and oversight by the Independent Group Advising on the Release of Data (IGARD). Organisations approved to use this data will be required to enter into a data sharing agreement with NHS Digital regulating the use of the data.
There are a number of organisations who are likely to need access to different elements of patient data from the General Practice Data for Planning and Research collection. These include but may not be limited to:
- the Department of Health and Social Care and its executive agencies, including Public Health England and other government departments
- NHS England and NHS Improvement
- primary care networks (PCNs), clinical commissioning groups (CCGs) and integrated care organisations (ICOs)
- local authorities
- research organisations, including universities, charities, clinical research organisations that run clinical trials and pharmaceutical companies
If the request is approved, the data will either be made available within a secure data access environment within NHS Digital infrastructure, or where the needs of the recipient cannot be met this way, as a direct dissemination of data. We plan to reduce the amount of data being processed outside central, secure data environments and increase the data we make available to be accessed via our secure data access environment. For more information read about improved data access in improving our data processing services.
Data will always be shared in the uniquely coded form (de-personalised data in the diagram above) unless in the circumstances of any specific request it is necessary for it to be provided in an identifiable form (personally identifiable data in the diagram above). For example, when express patient consent has been given to a researcher to link patient data from the General Practice for Planning and Research collection to data the researcher has already obtained from the patient.
It is therefore possible for NHS Digital to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason which permits this without breaching the common law duty of confidentiality. This would include:
- where the data was needed by a health professional for your own care and treatment
- where you have expressly consented to this, for example to participate in a clinical trial
- where there is a legal obligation, for example where the COPI Notices apply - see Our legal basis for collecting, analysing and sharing patient data above for more information on this
- where approval has been provided by the Health Research Authority or the Secretary of State with support from the Confidentiality Advisory Group (CAG) under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (COPI) - this is sometimes known as a ‘section 251 approval’
This would mean that the data was personally identifiable in the diagram above. Re-identification of the data would only take place following approval of the specific request through the Data Access Request Service, and subject to independent assurance by IGARD and consultation with the Professional Advisory Group, which is made up of representatives from the BMA and the RCGP. If you have registered a National Data Opt-out, this would be applied in accordance with the National Data Opt-out policy before any identifiable patient data (personally identifiable data in the diagram above) about you was shared. More about the National Data Opt-out is in the section below.
Details of who we have shared data with, in what form and for what purposes are published on our data release register.
Where NHS digital stores patient data
NHS Digital only stores and processes patient data for this data collection within the United Kingdom (UK).
Fully anonymous data (that does not allow you to be directly or indirectly identified), for example statistical data that is published, may be stored and processed outside of the UK. Some of our processors may process patient data outside of the UK. If they do, we will always ensure that the transfer outside of the UK complies with data protection laws
Talking Therapies services offer treatment for a wide range of common mental health problems such as (but not exclusively):
- Anxiety
- Stress
- Depression
- Obsessive compulsive disorder (OCD)
- Post-traumatic Stress Disorder (PTSD)
- Panic disorder
- Phobias
- Social Anxiety
- Health Anxiety
We offer a range of advice and treatment options, including signposting information, online self-help, cognitive behavioural therapy (CBT), eye-movement desensitisation therapy (EMDR) and referrals for other mental health or support services.
Referrals to NHS Talking Therapies are accepted via a person’s GP or other health professional. Alternatively people can contact the service and self-refer by calling us or visiting our website.
Doncaster: 03000 211556
Doncaster Long-Term Conditions: 0300 211563
Rotherham: 03000 215 108
North Lincs: 03000 216 165
This service is not a crisis service and operates from 9-5 Monday to Friday. If you feel you need immediate support, or are in danger, please contact one of the following:
- 999 or 111
- 116123 to reach the Samaritans for telephone contact
- text SHOUT to 85258 for crisis support via text
https://www.youtube.com/watch?v=jLgv0E1k6hs
NHS Talking Therapies – for anxiety and depression
(Previously named Improving Access to Psychological Therapies (IAPT) )
Swallownest Health Centre provides medical care to our registered patients according to a contract. This work is considered ‘NHS’ work and includes clinical appointments, vaccination appointments, chronic disease reviews, nurse appointments, certain minor surgical procedures, administration of hospital letters, monitoring of prescribed drugs.
We are also often asked to perform certain non-NHS work such as medical reports for employers, insurance reports, medicals for fostering/adoption agencies, DVLA reports and medicals. As this is work beyond our core contract it is something that the practice makes a charge for as it often requires quite time-consuming assessment which has to be done outside of our core medical services.
We undertake this work as we realise that it is difficult for our patients to get this private work completed elsewhere but it is not work we are contracted nor obliged to complete.
Below details our standard fees. It is important to remember that the fee is designed to reflect both the time taken to complete the work as well as the degree of risk that the GP takes on by making the declaration. It is also needed to cover the overhead costs and time taken for support staff to assist in the completion of this work.
Please be aware that you can seek to have this private work done elsewhere and it may be that you find more different prices with other providers. The fees we quote are based largely on BMA recommendations although some adjustments are made to reflect the time/risk that providing the work creates to the health centre.
Please note that pre-payment should be made for all work and please also note that private work may take up to 28 days
Service |
Standard Fee |
Who pays |
Payable to |
Additional notes |
To whom it may concern letters |
£30 |
Patient |
Swallownest Health Centre |
Dictated by GP and collected by patient |
Adoption/Fostering MedicalAH1 form |
£150 |
Local Authority/Fostering Agency |
The doctor completing report |
Add to waiting list |
Adoption/Fostering MedicalAH2 form |
£50 |
Local Authority/Fostering Agency |
The doctor completing report |
Add to waiting list |
Medical report for employer |
£150 |
Employer/Patient |
Swallownest Health Centre |
To GP who knows best/usual GP |
Cancellation of holiday claim form |
£50 |
Patient |
Swallownest Health Centre |
To GP who knows best/usual GP |
Firearm/shotgun license form |
£30 |
Patient |
Swallownest Health Centre |
|
D4 DVLA medical examination for a group 2 license |
£130 |
Patient |
The doctor completing form |
KT/AD both complete. Please task |
CN2EXAM DVLA form |
£85 |
DVLA |
Swallownest Health Centre |
Patient should book a GP exam, preferably with usual GP. Form completed at appt. |
Cremation form 4 |
£82 |
Funeral Home |
The doctor completing the form |
Doctor who has seen patient in 28 days before death. |
FAQs regarding why GPs have to charge for some services, provided by the British Medical Association (BMA)
- Surely the doctor is being paid anyway?
- It is important to understand that many GPs are not employed by the NHS.
- They are self-employed and they have to cover their costs - staff, buildings, heating, lighting, etc - in the same way as any small business.
- The NHS covers these costs for NHS work, but for non-NHS work, the fees charged by GPs contribute towards their costs.
- What is covered by the NHS and what is not?
- The Government’s contract with GPs covers medical services to NHS patients, including the provision of ongoing medical treatment.
- In recent years, however, more and more organisations have been involving doctors in a whole range of non-medical work.
- Sometimes the only reason that GPs are asked is because they are in a position of trust in the community, or because an insurance company or employer wants to ensure that information provided to them is true and accurate.
- Examples of non-NHS services for which GPs can charge their own NHS patients:
- accident or sickness certificates for insurance purposes
- fitness to attend school or university and holiday insurance certificates
- reports for health clubs to certify that patients are fit to exercise
- Examples of non-NHS services for which GPs can charge other institutions:
- life assurance and income protection reports for insurance companies
- reports for the Department for Work and Pensions (DWP) in connection with disability living allowance and attendance allowance
- medical reports for local authorities in connection with adoption and fostering
- Do GPs have to do non-NHS work for their patients?
- With certain limited exceptions, for example a GP confirming that one of their patients is not fit for jury service, GPs do not have to carry out non-NHS work on behalf of their patients.
- Whilst GPs will always attempt to assist their patients, they are not required to do such non-NHS work.
- Is it true that the BMA sets fees for non-NHS work?
- We suggest fees that GPs may charge their patients for non-NHS work (ie work not covered under their contract with the NHS) in order to help GPs set their own professional fees.
- However, the fees suggested by us are intended for guidance only; they are not recommendations and a doctor is not obliged to charge the rates we suggest.
- Can a fee be charged by a GP for the completion of cremation forms?
- It is important to differentiate between death certificates (which must be completed free of charge) and cremation forms.
- Cremation forms, unlike death certificates, require doctors to make certain investigations which do not form part of their NHS duties.
- A deceased person cannot be cremated until the cause of death is definitely known and properly recorded. Before cremation can take place two certificates need to be signed, one by the GP and one by another doctor.
- Cremation form 4 must be, as stated, completed by the registered medical practitioner who attended the deceased during their last illness.
- Form 5 must be completed by a registered medical practitioner who is neither a partner nor a relative of the doctor who completed form.
- A fee can be charged for the completion of both forms 4 and 5 as this does not form part of a doctor's NHS duties.
- Doctors normally charge these fees to the funeral director, who, generally passes on the cost to the family. Doctors are also entitled to charge a mileage allowance, where appropriate.
- The fees for cremation forms 4 and 5 (which are agreed with the National Association of Funeral Directors, NAFD, the National Society of Allied and Independent Funeral Directors, SAIF, and Co-operative Funeralcare) are available on our website.
- Why does it sometimes take my GP a long time to complete my form?
- Time spent completing forms and preparing reports takes the GP away from the medical care of his or her patients.
- Most GPs have a very heavy workload and paperwork takes up an increasing amount of their time, so many GPs find they have to take some paperwork home at night and weekends.
- I only need the doctor's signature - what is the problem?
- When a doctor signs a certificate or completes a report, it is a condition of remaining on the Medical Register that they only sign what they know to be true.
- In order to complete even the simplest of forms, therefore, the doctor might have to check the patient's entire medical record. Carelessness or an inaccurate report can have serious consequences for the doctor with the General Medical Council (the doctors' regulatory body) or even the Police.
- What will I be charged?
- We recommend that GPs tell patients in advance if they will be charged, and what the fee will be.
- It is up to individual doctors to decide how much they will charge, but we produce lists of suggested fees which many doctors use. Surgeries often have lists of fees on the waiting room wall based on these suggested fees.
- What can I do to help?
- Not all documents need a signature by a doctor, for example passport applications. You can ask another person in a position of trust to sign such documents free of charge.
- If you have several forms requiring completion, present them all at once and ask your GP if he or she is prepared to complete them at the same time to speed up the process.
- Do not expect your GP to process forms overnight. Urgent requests may mean that a doctor has to make special arrangements to process the form quickly, and this will cost more.
- What type of report work doesn't have to be done by my GP?
There is some medical examination and report work that can be done by any doctor, not only a patient's GP. For this work there are no set or recommended fees which means doctors may set their own fees. We offer guidelines only.
Your online mental wellbeing communities. Kooth and Quell offer Free, safe, and anonymous support and is here to support you through anything no matter how big or small. Information and sign up details can be found on the links below.
We are proud to have joined up with Rother Valley Parkrun. Come and join us on Saturday mornings from 9:00am and reap the benefits of fresh air, exercise and friendship. All for free! No appointments or prescriptions necessary.
Please click on the link for more information https://www.parkrun.org.uk/rothervalley/
- NHS Talking Therapies – for anxiety and depression (rdash.nhs.uk) IAPT Rotherham, also talking therapies.
- Home - Qwell a new online and completely confidential support service for those with MH ailments. Some patients have stated they have been provided counselling through this service as an additional support.
- ieso Online Therapy | Rotherham (iesohealth.com) another alternates online MH support service.
- Home | Rotherham & Barnsley Mind (rbmind.co.uk) supporting those with MH through counselling and therapies although there can be a fee.
- Rotherham Mental Health Support | Teladoc myStrength this one is a new one to me so I can’t offer patient feedback, seemingly an app that can be downloaded and used.
- Protecting Vulnerable Adults – Safer Rotherham Partnership support to protect vulnerable individual.
- Support Agencies and Helplines - Rotherham Abuse Counselling Service (rothacs.org.uk) This website has links to services such as Action housing, rush house, victim support, children, and young people services etc. A wide array supporting vulnerable homeless, children, DA victims.
- FUNCTIONAL FITNESS | Exercise | ENGLAND (functionalfitnesstrx.co.uk) supporting people who have or recovered from physical health ailments such as cancer, arthritis, COPD, Parkinson’s, mobility issues. Support in maintaining or managing physical health.
- Sheffield ME and Fibromyalgia Group | England (sheffieldmegroup.co.uk) support for those with fibromyalgia. Online and in person community support
- Working Win - Referral Form (workingwinreferrals.co.uk) support for those with physical and mental health conditions, help to find meaningful and sustainable employment.
- Home - Crossroads Care Rotherham (crossroadsrotherham.co.uk) a non-profit organisation supporting carers and those cared for.
- IAPT Long Term Conditions – RDaSH NHS Foundation Trust IAPT LTHC support
What is a PPG?
A Patient Participation Group (PPG) is a patient led group of volunteers who meet regularly. It is a forum to work together with their GP practice to help plan and improve services, offering a patients or carers views on the health services available to them.
What a PPG is not!
The PPG is not a forum to deal with personal medical issues and complaints, any individual concerns should be taken to the Practice Manager. Personal medical issues should be discussed with the Doctor or Nurse who is treating that patient, and not discussed at meetings. PPG/VPPG members should not provide any medical advice to other patients. Ground rules, and codes of contact should clearly state how these issues can be handled during meetings.
The purpose of a PPG is to
- Give patients and practice staff the opportunity to meet and discuss topics of shared interest, acting as a ‘critical friend’
- Support patients to get involved, and to make suggestions about the services they receive
- Constructively consider issues and to monitor themes that emerge from patient feedback. This could be from comments, complaints, surveys; online forums and the Friends and Family Test feedback.
- Contribute to action plans and support improvements
- Support health awareness, patient education, activities and campaigns, such as healthy eating or flu vaccination events
- Help the practice reach out to less heard parts of the practice population
- As each PPG develops, they will decide together what they want to do, and each will of course be different.
- PPGs can be incredibly helpful in developing, designing and carrying out patient surveys; supporting events; and checking that patient information is understandable, both in leaflets and on the website.
Who?
A PPG is open to every patient registered with the practice; this is the only membership requirement.
We meet every 2-3 months for an hour to discuss. If you would like to come along to the meeting, or if you have any questions please contact the surgery on 0114 4333888 or email [email protected] Please refer to the meeting notes for dates of the next and future meetings.
PPG Minutes
PPG Meeting Minutes 09.02.2024
PPG - Patient Participation Group - Additional Boundary Meeting 26.05.2023
PPG Minutes 20220729 - Presentation
PPG Minutes 20220401 - Presentation
PPG Minutes 20220218 - Presentation
PPG Minutes 20211210 - Presentation
PPG Minutes 20210611 - Presentation
PPG/AGM Minutes 20210428 - Presentation
PPG Minutes 20210226 - Presentation
PPG Minutes 20210129 - Presentation - Letter 100121 - Letter 120112
PPG Minutes 20201218- Presentation
PPG Minutes 20201023 - Presentation
PPG Minutes 20200904 - Presentation
Confidentiality & Medical Records
The practice complies with data protection and access to medical records legislation. Identifiable information about you will be shared with others in the following circumstances:
- To provide further medical treatment for you e.g. from district nurses and hospital services.
- To help you get other services e.g. from the social work department. This requires your consent.
- When we have a duty to others e.g. in child protection cases anonymised patient information will also be used at local and national level to help the Health Board and Government plan services e.g. for diabetic care.
If you do not wish anonymous information about you to be used in such a way, please let us know.
Reception and administration staff require access to your medical records in order to do their jobs. These members of staff are bound by the same rules of confidentiality as the medical staff.
Confidentiality & Young People
All patients have the right to confidentiality and privacy regarding their conversations with health professionals and have the right be seen without parents or guardians being present. If you wish to speak to a doctor or a nurse in private plase tell them and they will make sure you are seen on your own.
Freedom of Information
Information about the General Practioners and the practice required for disclosure under this act can be made available to the public. All requests for such information should be made to the practice manager.
Access to Records
In accordance with the Data Protection Act 1998 and Access to Health Records Act, patients may request to see their medical records. Such requests should be made through the practice manager and may be subject to an administration charge. No information will be released without the patient consent unless we are legally obliged to do so.
Complaints
We make every effort to give the best service possible to everyone who attends our practice.
However, we are aware that things can go wrong resulting in a patient feeling that they have a genuine cause for complaint. If this is so, we would wish for the matter to be settled as quickly, and as amicably, as possible.
To pursue a complaint please contact the practice manager who will deal with your concerns appropriately. Further written information is available regarding the complaints procedure from reception. Constructive criticism and compliments are always welcome and can be posted to the NHS Choices website by following the link.
Zero Tolerance Policy
The NHS operate a zero tolerance policy with regard to violence and abuse and the practice has the right to remove violent patients from the list with immediate effect in order to safeguard practice staff, patients and other persons. Violence in this context includes actual or threatened physical violence or verbal abuse which leads to fear for a person’s safety. In this situation we will notify the patient in writing of their removal from the list and record in the patient’s medical records the fact of the removal and the circumstances leading to it.
The more you know about your pregnancy and your options, the more you are likely to feel in control. The information given here is based on The Pregnancy Book, which your midwife should give you at your first appointment.
Before you are pregnant
Your pregnancy and labour
- 37-40 weeks pregnantHow the baby develops
- 0-8 weeks pregnant
- 9-12 weeks pregnant
- 13-16 weeks pregnant
- 17-20 weeks pregnant
- 21-24 weeks pregnant
- 25-28 weeks pregnant
- 29-32 weeks pregnant
- 33-36 weeks pregnant
- 40+ weeks pregnant
- Your health in pregnancy
- Common health problems
- Antenatal care and classes
- Choosing where to have your baby
- Labour and birth
- When pregnancy goes wrong
You and your baby
General pregnancy topics
Primary Care Network (PCN)
Patient Information
Which Practices are a part of the Rother Valley South PCN?
Dinnington Group Practice
Kiveton Medical Centre
Swallownest Health Centre
The Village Surgery
What is a Primary Care Network?
A Primary Care Network consists of groups of general practices working together with a range of local providers, including across Primary Care, community services, social care and the voluntary sector, to offer more personalised, coordinated health and social care to their local populations. Networks will normally be based around natural local communities typically serving populations of at least 30,000 and not tending to exceed 50,000.
They should be small enough to maintain the traditional strengths of general practice but at the same time large enough to provide resilience and support the development of integrated teams.
Rother Valley South PCN
Rother Valley South PCN have a collective patient population circa 57,000 and we believe we are the optimum size to enable us to continue to work effectively together and improve patient services and health outcomes.
What are PCN's designed to do?
Primary Care Networks will provide proactive, coordinated care to their local population, in different ways to match different people's needs, with a strong focus on prevention and personalised care. This means supporting patients to make informed decisions about their own health and care and connecting them to a wide range of statutory and voluntary services to ensure they can access the care they need first time.
Networks will also have a greater focus on population health and addressing health inequalities in their local area, using data and technology to inform the delivery of population scale care models.
Primary Care Networks will also help ensure that the NHS designs support and services to get the best possible value out of their funding for their local communities.
We will be working alongside :-
- Clinical Pharmacists
- Social Prescribers
- Paramedics
to deliver a holistic approach to healthcare, with a strong focus on prevention and personalised care.
Our Aims
- To work at scale, efficiently and effectively in order to deliver Primary Health Care to the patients registered with each member Practice.
- To deliver New Models of Care, incorporating the GP Five Year Forward View, 10 high impact actions to release capacity in general practice.
- To develop a suitably qualified skill mixed workforce fit to take the NHS into 2020 and beyond
- To listen to the views of our patient population in order to provide the most appropriate access to services.
- To work together to ensure we provide good care for both patient and staff whilst continuing to maintain the independence and individuality of each practice.
NB For the foreseeable future there will be no changes to practice staff and their current roles. Staff and patients are an invaluable and important part of this process and will be kept informed and involved at all times. Practices will continue to operate as they do currently and patients may see some changes. Patients will be kept informed of any changes at all times.
DATA PROTECTION - GDPR
During the course of our work we may share your information with these practices and health care organisations / professionals. We will only share this information where it relates to your direct healthcare needs.
When we do this, we will always ensure that appropriate agreements are in place to protect your information and keep it safe and secure. This is also what the Law requires us to do. If you would like to see the information the PCN holds about you please contact the Practice Data Protection Officer
Any other queries on the PCN can be directed to the Practice Manager at the surgery or contact the PCN Clinical Director, Dr T J Douglas, GP Partner, Dinnington Group Practice
To report an issue with our website please use this form.
RotherHive provides a range of verified practical Mental Health and Wellbeing Information, Support and Advice for adults in Rotherham
www.rotherhive.co.uk
Have you heard about Rotherham Gismo, the online directory of not-for-profit groups providing help and support to people living and working in the area. The site features around 600 groups offering a wide range of support services to individuals in the community. Each group has its own page to explain their aims and highlight the various services and activities they provide.
The site has information from an extensive range of groups in the area so its easy for you discover who is doing WHAT and WHERE and WHEN.
Find local groups and the range of activities they organise.
Find support services to help you, your family and friends.
Find groups which will help you keep active or learn new skills
Find a range of activities taking place in the coming weeks.
Find out how you can help others by volunteering your time.
We are excited to announce that Rotherham Healthwave is now live! https://rotherham-healthwave.connecthealthcarerotherham.co.uk/
Looking to lose weight, improve wellbeing or quit smoking?
Self-refer on our website today and start your journey to a healthier, happier you.
Look out for group sessions at Swallownest Health Centre soon!
Risk Profiling: how your NHS records are used
Privacy Notice
This practice is taking part in a new NHS service that helps your family Doctor (GP) to spot whether you need more help to manage your health. The service is called "risk profiling".
Using information from your health records, a secure NHS computer system will look at any recent treatments you have had in hospital or at this surgery, and any existing health conditions that you have, and alert your Doctor to the likelihood of a possible future hospital admission. The clinical Risk Stratification in General Practice team at the surgery will use the information to help you get early care and treatment where it is needed. The information will be seen only by qualified health workers involved in your care. NHS security systems will protect your health information and patient confidentiality at all times.
If you don't want your information being used in this way, or have any other concerns, please contact Miss Sarah Buckley, Practice Manager ([email protected])
What is Sepsis?
Sepsis is when your body fights too hard against infection. Sometimes important organs will get damaged.
If not treat quickly, Sepsis can cause death.
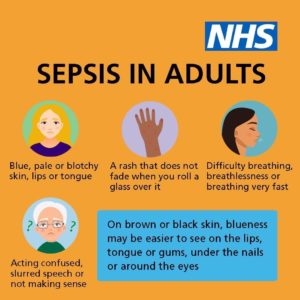

SPOT ANY SIGNS OF SEPSIS? CALL 999 OR GO TO A&E
1 in 4 people in the UK will experience a mental health problem each year. IAPT can offer a range of local therapies that can help with stress, anxiety, and depression. Giving people the right information and help to develop skills to overcome stress, anxiety and depression is at the heart of what IAPT do. Please take some time to look at the information on the IAPT website that we hope will help guide you to the right therapy for you. You will find information on self-help and a range of activities and support available in your local area, as well as a range of therapies that we can offer including help online Telephone: 0114 2264380
We believe it’s the right of every young carer to be recognised in their role and have the same opportunities as other children and young people of a similar age.
Our practice participates in the training of Medical Students on behalf of Sheffield University Medical School.
There is a new Central NHS Computer System called the Summary Care Record (SCR). It is an electronic record which contains information about the medicines you take, allergies you suffer from and any bad reactions to medicines you have had.
Why do I need a Summary Care Record?
Storing information in one place makes it easier for healthcare staff to treat you in an emergency, or when your GP practice is closed.
This information could make a difference to how a Doctor decides to care for you, for example which medicines they choose to prescribe for you.
Who can see it?
Only healthcare staff involved in your care can see your Summary Care Record.
How do I know if I have one?
Over half of the population of England now have a Summary Care Record. You can find out whether Summary Care Records have come to your area by looking at our interactive map or by asking your GP
Do I have to have one?
No, it is not compulsory. If you choose to opt out of the scheme, then you will need to complete a form and bring it along to the surgery. You can use the form at the foot of this page.
More Information
For further information visit the NHS Care records website
- Welcome to Age UK Rotherham age UK Rotherham, befriending, finance, isolation, community groups/access and many more.
- b:friend | Let's end loneliness together, let's b:friend (letsbfriend.org.uk) A face to face or telephone befriending service.
- Rotherham Community Transport | Door 2 Door | Shopper Bus | Dial a Ride specialised community transport.
- Refer to Single Point of Access | Instructions – Rotherham Metropolitan Borough Council single point of access for any concerns around those living alone, social support of home adaptations.
- Aston Community Library and Customer Service Centre | Accessible SWALLOWNEST library blue badge application support as it is now digital, these help non-digital users apply.
Our practice has been approved to trial for the next 6 months as a veteran friendly practice, please find attached some information regarding this service.