As a practice, we are fully committed to the sustainability and reduction of our carbon footprint. We have signed up to being a ‘Greener Practice’ and will be working with both our staff and patients to improve our carbon footprint.
Green Inhaler
For many people with lung disease, inhalers are a lifeline; allowing you to take control of breathing problems and open up your airways. So it can come as a shock to learn that some inhalers come with a large carbon footprint. The most commonly used inhaler in the UK for instance, Ventolin Evohaler™, has a carbon footprint equivalent to 28kg of CO2. Many patients are now seeking ways to reduce the greenhouse gas released from their inhalers. For some, switching inhalers could save as much greenhouse gas as becoming vegetarian.
Equivalent tailpipe greenhouse gas emissions from a Ventolin Evohaler (containing 100 2-puff doses) and a Ventolin Accuhaler (60 1-puff doses). Assumes car achieves 100gCO2/km.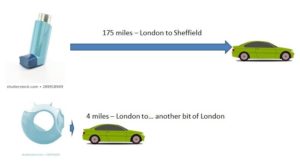
Before making any changes to your treatment you should consult a healthcare professional. Stopping your inhaler because of its carbon footprint is not recommended, not least because if you have an exacerbation the extra treatment you need could greatly increase your carbon footprint!
This site will show you why some inhalers have such a large carbon footprint and will outline some ways to reduce it. Some patients may be able to switch inhalers, but the most important thing is to keep your disease under control. If you do need an inhaler containing greenhouse gases please don’t feel guilty – everyone has a carbon footprint. There are still things you can do to reduce the carbon footprint of your inhalers, and the pharmaceutical industry is working hard to develop new propellants with a much smaller carbon footprint.
The Named GP is largely a role of oversight. It reassures patients they have one GP who is responsible for their care.
- Patients do not need to see their named GP when they book an appointment with the practice.
- Patients are entitled to choose to see any GP or nurse in the practice but please be aware you may have to wait longer.
- The named GP works with relevant health and social care professionals to deliver a multidisciplinary care package that meets the needs of the patients.
- The named GP ensures that these patients have access to a health check
- The named GP will NOT take on 24hr responsibility for the patient.
Losing a baby can be an unbelievably painful and traumatic experience.
That's why parents who have lost a baby before 24 weeks of pregnancy in England can now apply for an official baby loss certificate.
This is a voluntary service we’re introducing as part of the #WomensHealthStrategy and #PregnancyLossReview to support grieving parents and acknowledge their pain.
Information on eligibility and how to apply: https://www.gov.uk/request-baby-loss-certificate
Our practice does not offer a Blue Badge completion service, if you have been asked for supporting professional information, please contact your specialist. Blue badge parking permits – Rotherham Metropolitan Borough Council
Our Practice does not offer a Fit2Fly form/certificate completion service they can be obtained through a Private GP service.
Swallownest Health Centre provides medical care to our registered patients according to a contract. This work is considered ‘NHS’ work and includes clinical appointments, vaccination appointments, chronic disease reviews, nurse appointments, certain minor surgical procedures, administration of hospital letters, monitoring of prescribed drugs.
We are also often asked to perform certain non-NHS work such as medical reports for employers, insurance reports, medicals for fostering/adoption agencies, DVLA reports and medicals. As this is work beyond our core contract it is something that the practice makes a charge for as it often requires quite time-consuming assessment which has to be done outside of our core medical services.
We undertake this work as we realise that it is difficult for our patients to get this private work completed elsewhere but it is not work we are contracted nor obliged to complete.
Below details our standard fees. It is important to remember that the fee is designed to reflect both the time taken to complete the work as well as the degree of risk that the GP takes on by making the declaration. It is also needed to cover the overhead costs and time taken for support staff to assist in the completion of this work.
Please be aware that you can seek to have this private work done elsewhere and it may be that you find more different prices with other providers. The fees we quote are based largely on BMA recommendations although some adjustments are made to reflect the time/risk that providing the work creates to the health centre.
Please note that pre-payment should be made for all work and please also note that private work may take up to 28 days
After careful consideration the practice has decided to no longer prescribe diazepam for patients having MRI scans or other investigative procedures. We have a duty of care to provide safe, consistent, and appropriate care for our patients.
Please see the reasons outlined below to explain our concerns.
- Small doses of diazepam may be sub-therapeutic for most adults for any effective sedation. Although diazepam makes most people who take it sleepy, in some rare situations it can have the opposite effect and make people aggressive or agitated. This may result in your procedure being delayed.
- A patient may take a sedative an hour before their assumed procedure, to then attend the hospital and find that the procedure has been delayed, therefore the timing of the anxiolytic being sub optimal.
- GP’s are not regularly involved, skilled, or trained to provide the correct level of sedation for a procedure/scan.
- It is the responsibility of the hospital consultants/doctor requesting the imaging to prescribe medication if they deem necessary. They can do this through the hospital pharmacy or organising a prescription themselves.
- Sedated patients should be monitored regularly for any adverse effects of the medication.
- The Royal College of Radiologists’ own guidelines on sedation for imaging makes no mention of GP involvement or provision of low dose anxiolytics and stresses the importance of experienced well-trained staff involved and the monitoring of sedated patients.
We would be grateful if you could discuss this with the relevant specialist who has requested this, and to prescribe as they see fit.
Thank you,
The Partners at Swallownest Health Centre
January 2024
Primary Care Network (PCN)
Patient Information
Which Practices are a part of the Rother Valley South PCN?
Dinnington Group Practice
Kiveton Medical Centre
Swallownest Health Centre
The Village Surgery
What is a Primary Care Network?
A Primary Care Network consists of groups of general practices working together with a range of local providers, including across Primary Care, community services, social care and the voluntary sector, to offer more personalised, coordinated health and social care to their local populations. Networks will normally be based around natural local communities typically serving populations of at least 30,000 and not tending to exceed 50,000.
They should be small enough to maintain the traditional strengths of general practice but at the same time large enough to provide resilience and support the development of integrated teams.
Rother Valley South PCN
Rother Valley South PCN have a collective patient population circa 57,000 and we believe we are the optimum size to enable us to continue to work effectively together and improve patient services and health outcomes.
What are PCN's designed to do?
Primary Care Networks will provide proactive, coordinated care to their local population, in different ways to match different people's needs, with a strong focus on prevention and personalised care. This means supporting patients to make informed decisions about their own health and care and connecting them to a wide range of statutory and voluntary services to ensure they can access the care they need first time.
Networks will also have a greater focus on population health and addressing health inequalities in their local area, using data and technology to inform the delivery of population scale care models.
Primary Care Networks will also help ensure that the NHS designs support and services to get the best possible value out of their funding for their local communities.
We will be working alongside :-
- Clinical Pharmacists
- Social Prescribers
- Paramedics
to deliver a holistic approach to healthcare, with a strong focus on prevention and personalised care.
Our Aims
- To work at scale, efficiently and effectively in order to deliver Primary Health Care to the patients registered with each member Practice.
- To deliver New Models of Care, incorporating the GP Five Year Forward View, 10 high impact actions to release capacity in general practice.
- To develop a suitably qualified skill mixed workforce fit to take the NHS into 2020 and beyond
- To listen to the views of our patient population in order to provide the most appropriate access to services.
- To work together to ensure we provide good care for both patient and staff whilst continuing to maintain the independence and individuality of each practice.
NB For the foreseeable future there will be no changes to practice staff and their current roles. Staff and patients are an invaluable and important part of this process and will be kept informed and involved at all times. Practices will continue to operate as they do currently and patients may see some changes. Patients will be kept informed of any changes at all times.
DATA PROTECTION - GDPR
During the course of our work we may share your information with these practices and health care organisations / professionals. We will only share this information where it relates to your direct healthcare needs.
When we do this, we will always ensure that appropriate agreements are in place to protect your information and keep it safe and secure. This is also what the Law requires us to do. If you would like to see the information the PCN holds about you please contact the Practice Data Protection Officer
Any other queries on the PCN can be directed to the Practice Manager at the surgery or contact the PCN Clinical Director, Dr T J Douglas, GP Partner, Dinnington Group Practice
Policy regarding requests from private providers to take blood tests
Swallownest Health Centre follows the following guidance regarding requests for blood tests to be done by a private provider:
If a patient has chosen to pay for private healthcare because
- their treatment is not available on the NHS or
- they do not wish to be treated on the NHS
they are responsible for paying for all costs, including tests, and the private provider is responsible for managing every aspect of their healthcare (unless the patient chooses to transfer back to the NHS at a later date to continue treatment).
For that reason, private providers should not be asking GPs to arrange any tests that they deem necessary, and intend to use, to make a diagnosis and recommend a course of treatment with.
It is the private provider’s responsibility to arrange tests for patients whose care they are managing, and the patient’s responsibility to pay for them.
Policy regarding requests from private providers to start or take over prescribing medication
In addition to the above policy, the practice cannot prescribe on behalf of private providers nor continue to supply prescriptions which have previously been supplied by the private provider. We are not permitted to have shared care protocols with private providers.
Private consultants wishing to transfer patients to NHS care should directly refer their patient to the appropriate NHS service who will reassess and, if appropriate, take over your treatment. At the point that your care has been taken over by an NHS service, a request may be made by the NHS service to share prescribing responsibility with the practice. Our practice pharmacists review and manage all such requests.
Screening tests carried out by private providers which have not been approved by the UK National Screening Committee
The practice supports the national guidance.
If you choose to have private screening tests or investigations that are not available or recommended by the NHS, you should ensure that you have the funds or insurance in place to cover the costs of any additional treatment or investigation that is incurred as the NHS may not cover these.
Post Bariatric Surgery Follow-up of Private Patients
Where patients have procured their surgery in the private sector, the commissioners suggest that patients are advised of the need to ensure private follow-up.
- The first 2 years of post-operative care should be purchased in advance of having surgery, as the NHS will not provide this care.
- In addition, GPs be aware that as this is commissioned work, it potentially falls outside the cover of the Clinical Negligence Scheme for General Practice (CNSGP).
- GPs will only be covered for the instigation of investigations where a patient falls ill, rather than for routine monitoring.
Have you heard about Rotherham Gismo, the online directory of not-for-profit groups providing help and support to people living and working in the area. The site features around 600 groups offering a wide range of support services to individuals in the community. Each group has its own page to explain their aims and highlight the various services and activities they provide.
The site has information from an extensive range of groups in the area so its easy for you discover who is doing WHAT and WHERE and WHEN.
Find local groups and the range of activities they organise.
Find support services to help you, your family and friends.
Find groups which will help you keep active or learn new skills
Find a range of activities taking place in the coming weeks.
Find out how you can help others by volunteering your time.
What is Sepsis?
Sepsis is when your body fights too hard against infection. Sometimes important organs will get damaged.
If not treat quickly, Sepsis can cause death.
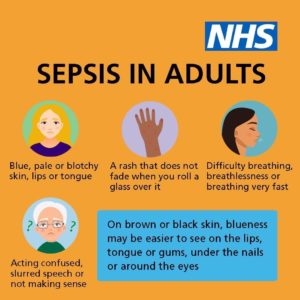

SPOT ANY SIGNS OF SEPSIS? CALL 999 OR GO TO A&E
When you attend for a test of any kind you should be told that you will be contacted if the results need following up. If you sign up for online services you will be able to check your own results on-line at any time, as soon as they have been checked by a Doctor. You will also be able to compare them with previous results in your notes.
Please do not assume "no news is good news" in case the result has gone astray or we have tried and failed to reach you.
Most blood tests results are back in a few working days, but some tests, especially rarer ones may take longer. Just because one result is back, it does not mean they are all back. Most x-ray results are back within 7-10 days, but if a test suggests something serious, it is likely we will be told more quickly.
Our reception staff are not qualified to explain any results: they can only repeat the brief comment that the Doctor has attached to the results, such as "normal" or "make appointment". Sometimes if the result is particularly sensitive (e.g. HIV test) or complicated, the Doctor will recommend receiving the result in person.
Normally results are sent to the Doctor who ordered the test. If a hospital Doctor orders a test, the GP may not receive the result and may even not know it has been done. You can contact the specialist's secretary to ask about results, although usually a hospital secretary will not provide a result directly- the secretary may ask a hospital Doctor to phone you back or they may involve the GP. Routine hospital letters can take up to a month to reach us, sometimes longer.
Medical Examiner Information for Members of the Public
The law in England and Wales is changing and from 9th September 2024 all deaths will need to be reviewed by a Medical Examiner if not by a Coroner.
Who are Medical Examiners and Medical Examiner Officers, and what do they do?
Medical Examiners are independent senior medical doctors who come from a variety of medical specialities. They review all hospital deaths and also those occurring at home, in care home, hospices and other community settings. They are supported in this role by Medical Examiner Officers. Both Medical Examiner and Medical Examiner Officer have undertaken specialist training for this role from the Royal College of Pathology.
Their job is to review the patient’s last care episode and ensure that their cause of death is recorded accurately. They do this by reviewing their medical records and also discussing with the doctors who looked after them. Medical Examiners also review the quality of care and make sure that it was satisfactory. Where there are concerns about the quality of care, or the death needs investigating further, the Medical Examiner Office will refer the case to an appropriate person to undertake this work, such as a Coroner.
A Medical Examiner or Medical Examiner Officer will contact the relative or representative of the person who died. This will usually be through a telephone call, or sometimes a meeting. This is quite routine and there is no cause for concern. They will discuss the Medical Examiner’s review and explain what is written on the Medical Certificate of Cause of Death and why, and check if you have any questions or concerns about the care the person received before their death. They can explain what medical language means, and make it easier to understand what happened.
You can be confident that Medical Examiners and Medical Examiner Officers will provide an independent view. They will never look into the causes of death of a person they personally provided care for. The Medical Examiner Office reports themes and concerns and provides information on public health surveillance. Any feedback that you can provide is incredibly important and will help the NHS provide better care for other patients and carers in future; for example, by identifying ways in which patient and family care could be improved.
Coroners
Some deaths, for example unexpected deaths, are notified to a Coroner who may decide to carry out their own independent investigation. This link explains more about Coroners and the types of deaths they investigate.
https://www.gov.uk/government/publications/notification-of-deaths-regulations-2019-guidance
The Medical Examiner may sometimes give the Coroner medical advice in these cases, but Coroners lead these investigations and Medical Examiners will not be directly involved. We can help answer questions about the steps and procedures involved when a case is referred to the Coroner.
Frequently Asked Questions about the Medical Examiner Process
What happens upon the death of a family member?
The Doctor that last attended to the deceased will complete a Medical Certificate of Cause of Death (MCCD). This document will be sent to the Medical Examiner electronically . The Medical Examiner will review the patients medical records, speak to family members, and make the decision to approve or contest the Cause of Death cited by the Doctor on the Certificate. Once the Medical Examiner has approved the MCCD, the certificate will be forwarded, again electronically, to the local Register Office.
When can I start the process of Arranging a funeral?
Funeral plans should not be confirmed until the Medical Examiner has conducted their review. All deaths must be registered at the Register Office by an informant – usually a relative. You can only book an appointment at the Register Office once the approved Medical Certificate of Cause of Death (MCCD) has been sent to the Register Office. Further information on the registration of deaths in the Rotherham area, including how to book an appointment, can be found at the Register Office – Rotherham Metropolitan Borough Council website. Only once both the Medical Examiner and Register Office processes have been completed, can the body be released
Will funeral plans or release of the body take longer?
We will be unable to issue Death Certificates or Cremation Certificates to family members, the Register Office or Funeral Directors, until the Medical Examiner has confirmed to us that their process is complete and that we are able to issue these documents. Medical Examiner offices make every effort to avoid any delays and work with families and carers of the person who died to meet the legal requirements for registering deaths. There will usually not be any additional delays incurred by this process and they will try to be flexible, for example where relatives would like the body to be released quickly for religious requirements. Please let the Doctor know if you wish for the process to be treated as Urgent.
Can I ask the Medical Examiner to talk to someone else if it’s too difficult for me to talk to them?
Yes, of course. Please let the Doctor who cared for the person know if you would like someone other than you to be the first point of contact. The Medical Examiner office will usually phone you around the time that the Medical Certificate of Cause of Death is being completed – but they can arrange another way of contacting you if you let us know what you prefer.
What if I don’t want to talk to the Medical Examiner office, or I don’t want to tell them about my concerns?
We understand this is likely to be a difficult time for you and it is your choice whether you talk to the Medical Examiner office or not. If you are not sure, you can contact the Medical Examiner office by calling the Rotherham Medical Examiner Service (details below) and request more information before deciding if you want to go ahead – they are trained to help bereaved people and will be very understanding.
Medical Examiner offices provide an independent view, so if you can, we encourage you to talk to them. They can explain things to you and are specially trained to answer your questions and act upon any concerns that you may have. If you don’t wish to talk to the Medical Examiner, please tell the patient’s doctor or the Medical Examiner when they call.
What can I do if I have concerns about the Medical Examiner process?
If you are not satisfied with the Medical Examiner office’s advice, please first discuss this with staff in the Medical Examiner Office, and if you are still not satisfied, you can also contact the Rotherham Hospital Patient Advice and Liaison Service on 01709 424461 or by emailing your.experience@nhs.net
How can I contact the Medical Examiner office?
The Medical Examiner office will contact you in the first instance. However, if your query is urgent, you can contact the Medical Examiner office:
01709 424465